Borderline personality disorder (BPD) is a psychological disorder characterized bya prolonged disturbance of personality accompanied by moods wings, unstable personal relationships, identity problems, threats of self-destructive behavior, fears of abandonment, and impulsivity. BPD is widely diagnosed—up to 20% of psychiatric patients are given the diagnosis, and it may occur in up to 2% of the general population (Hyman, 2002). 1About three quarters of diagnosed cases of BDP are women.
People with BPD fear being abandoned by others. They often show a clinging dependency on the other person and engage in manipulation to try to maintain the relationship. They become angry if the other person limits the relationship, but also deny that they care about the person. As a defense against fear of abandonment, borderline people are compulsively social. But their behaviors, including their intense anger, demands, and suspiciousness, repel people.
People with BPD often deal with stress by engaging in self-destructive behaviors, for instance by being sexually promiscuous, getting into fights, binge eating and purging, engaging in self- mutilation or drug abuse, and threatening suicide. These behaviors are designed to call forth a “saving” response fr om the other person. People with BPD are a continuing burden for police, hospitals, and therapists. Borderline individuals also show disturbance in their concepts of identity: They are uncertain about self-image, gender identity, values, loyalties, and goals. They may have chronic feelings of emptiness or boredom and be unable to tolerate being alone.
BPD has both genetic as well as environmental roots. In terms of genetics, research has found that those with BPD frequently have neurotransmitter imbalances (Zweig-Frank et al., 2006), 2 and the disorder is heritable (Minzenberg, Poole, & Vinogradov, 2008). 3 In terms of environment, many theories about the causes of BPD focus on a disturbed early relationship between the child and his or her parents. Some theories focus on the development of attachment in early childhood, while others point to parents who fail to provide adequate attention to the child’s feelings. Others focus on parental abuse (both sexual and physical) in adolescence, as well as on divorce, alcoholism, and other stressors (Lobbestael & Arntz, 2009). 4 The dangers of BPD are greater when they are associated with childhood sexual abuse, early age of onset, substance abuse, and aggressive behaviors. The problems are amplified when the diagnosis is comorbid (as it often is) with other disorders, such as substance abuse disorder, major depressive disorder, and posttraumatic stress disorder (PTSD; Skodol et al., 2002). 5
Research Focus: Affective and Cognitive Deficits in BPD
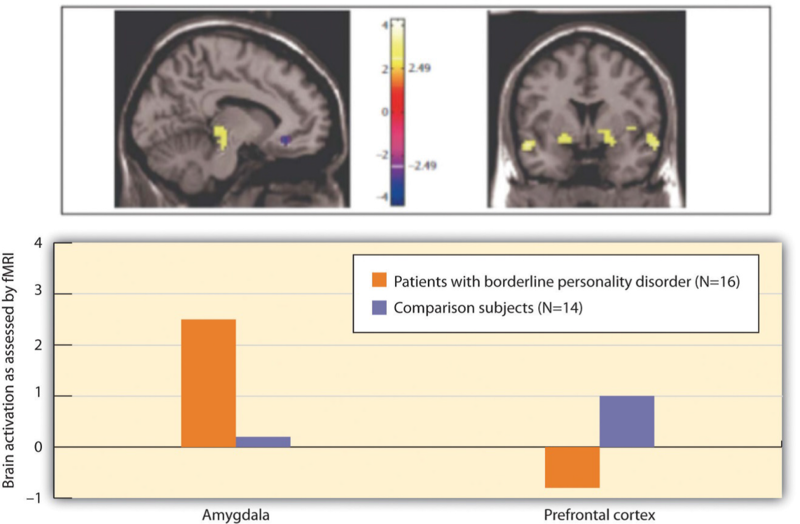
Posner et al. (2003) 6 hypothesized that the difficulty that individuals with BPD have in regulating their lives (e.g., in developing meaningful relationships with other people) may be due to imbalances in the fast and slow emotional pathways in the brain. Specifically, they hypothesized that the fast emotional pathway through the amygdala is too active, and the slow cognitive-emotional pathway through the prefrontal cortex is not active enough in those with BPD.
The participants in their research were 16 patients with BPD and 14 healthy comparison participants. All participants were tested in a functional magnetic resonance imaging (fMRI) machine while they performed a task that required them to read emotional and nonemotional words, and then press a button as quickly as possible whenever a word appeared in a normal font and not press the button whenever the word appeared in an italicized font.
The researchers found that while all participants performed the task well, the patients with BPD had more errors than the controls (both in terms of pressing the button when they should not have and not pressing it when they should have). These errors primarily occurred on the negative emotional words.
Figure 12.16 "Results From Posner et al., 2003" shows the comparison of the level of brain activity in the emotional centers in the amygdala (left panel) and the prefrontal cortex (right panel). In comparison to the controls, the borderline patients showed relatively larger affective responses when they were attempting to quickly respond to the negative emotions, and showed less cognitive activity in the prefrontal cortex in the same conditions. This research suggests that excessive affective reactions and lessened cognitive reactions to emotional stimuli may contribute to the emotional and behavioral volatility of borderline patients.
- 5188 reads