Thousands of studies have been conducted to test the effectiveness of psychotherapy, and by and large they find evidence that it works. Some outcome studies compare a group that gets treatment with another (control) group that gets no treatment. For instance, Ruwaard, Broeksteeg, Schrieken, Emmelkamp, and Lange (2010) 1 found that patients who interacted with a therapist over a website showed more reduction in symptoms of panic disorder than did a similar group of patients who were on a waiting list but did not get therapy. Although studies such as this one control for the possibility of natural improvement (the treatment group improved more than the control group, which would not have happened if both groups had only been improving naturally over time), they do not control for either nonspecific treatment effects or for placebo effects. The people in the treatment group might have improved simply by being in the therapy (nonspecific effects), or they may have improved because they expected the treatment to help them (placebo effects).
An alternative is to compare a group that gets “real” therapy with a group that gets only a placebo. For instance, Keller e t al. (2001) 2 had adolescents who were experiencing anxiety disorders take pills that they thought would reduce anxiety for 8 weeks. However, one-half of the patients were randomly assigned to actually receive the antianxiety drug Paxil, while the other half received a placebo drug that did not have any medical properties. The researchers ruled out the possibility that only placebo effects were occurring because they found that both groups improved over the 8 weeks, but the group that received Paxil improved significantly more than the placebo group did.
Studies that use a control group that gets no treatment or a group that gets only a placebo are informative, but they also raise ethical questions. If the researchers believe that their treatment is going to work, why would they deprive some of their participants, who are in need of help, of the possibility for improvement by putting them in a control group?
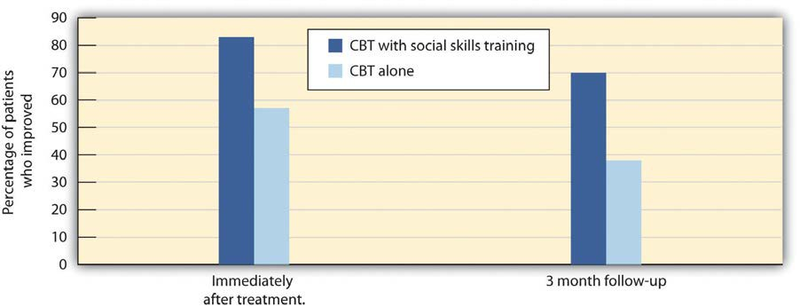
Another type of outcome study compares different approaches with each other. For instance, Herbert et al. (2005) 3 tested whether social skills training could boost the results received for the treatment of social anxiety disorder with cognitive-behavioral therapy (CBT) alone. As you can see in Figure 13.11, they found that people in both groups improved, but CBT coupled with social skills training showed significantly greater gains than CBT alone.
Other studies (Crits-Christoph, 1992; Crits-Christoph et al., 2004) 4 have compared brief sessions of psychoanalysis with longer-term psychoanalysis in the treatment of anxiety disorder, humanistic therapy with psychodynamic therapy in treating depression, and cognitive therapy with drug therapy in treating anxiety (Dalgleish, 2004; Hollon, Thase, & Markowitz, 2002). 5 These studies are advantageous because they compare the specific effects of one type of treatment with another, while a llowing all patients to get treatment.
ResearchFocus:Meta-AnalyzingClinicalOutcomes
Because there are thousands of studies testing the effectiveness
of psychotherapy, and the independent and dependent variables in the studies vary widely, the results are often combined using a meta-analysis. A meta- analysis is a statistical technique that uses the results of existing studiesto integrate and draw conclusions about those studies. In one important meta-analysis analyzing the effect of psychotherapy, Smith,
Glass, and Miller (1980) 6 summarized studies that compared different types of therapy or that compared the effectiveness of therapy
against a control group. To find the studies, the researchers systematically searched computer databases and the reference sections of previous research reports to locate every study that met
the inclusion criteria. Over 475 studies were located, and these studies used over 10,000 research participants.
The results of each of these studies were systematically coded,
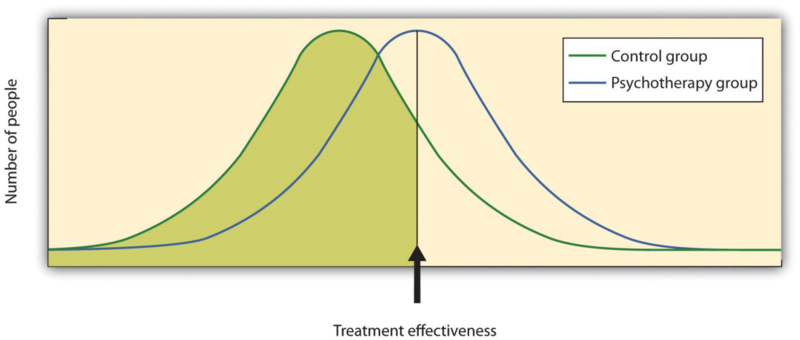
and a measure of the effectiveness of treatment known as the effect sizewas created for each study. Smith and her colleagues found that the average
effect size for the influence of therapy was 0.85, indicating that psychotherapy had a relatively large positive effect on recovery. What this means is that, overall, receiving psychotherapy
for behavioral problems is substantially better for the individual than no t receiving therapy (Figure 13.12 "Normal Curves of Those Who Do and Do Not Get Treatment"). Although they did not
measure it, psychotherapy presumably has large societal benefits as well—the cost of the therapy is likely more than made up for by the increased productivity of those who receive
it.
Other meta-analyses have also found substantial support for the effectiveness of specific therapies, including cognitive therapy, CBT (Butler, Chapman, Forman, & Beck, 2006; Deacon & Abramowitz, 2004), 7 couples and family therapy (Shadish & Baldwin, 2002), 8 and psychoanalysis (Shedler, 2010). 9 On the basis of these and other meta-analyses, a list ofempirically supportedtherapies—that is, therapies that are known to be effective—has been developed (Chambless & Hollon, 1998; Hollon, Stewart, & Strunk (2006). 10 These therapies include cognitive therapy and behavioral therapy for depression; cognitive therapy, exposure therapy, and stress inoculation training for anxiety; CBT for bulimia; and behavior modification for bed-wetting.
Smith, Glass, and Miller (1980) 11 did not find much evidence that any one type of therapy was more effective than any other type, and more recent meta-analyses have not tended to find many differences either (Cuijpers, van Straten, Andersson, & van Oppen, 2008). 12 What this means is that a good part of the effect of therapy is nonspecific, in the sense that simply coming to any type of therapy is helpful in comparison to not coming. This is true partly because there are fewer distinctions among the ways that different therapies are practiced than the theoretical differences among them would suggest. What a good therapist practicing psychodynamic approaches does in therapy is often not much different from what a humanist or a cognitive- behavioral therapist does, and so no one approach is really likely to be better than the other.
What all good therapies have in common is that they give people hope; help them think more carefully about themselves and about their relationships with others; and provide a positive, empathic, and trusting relationship with the therapist—the therapeutic alliance (Ahn & Wampold, 2001). 13 This is why many self-help groups are also likely to be effective and perhaps why having a psychiatric service dog may also make us feel better.
- 3649 reads