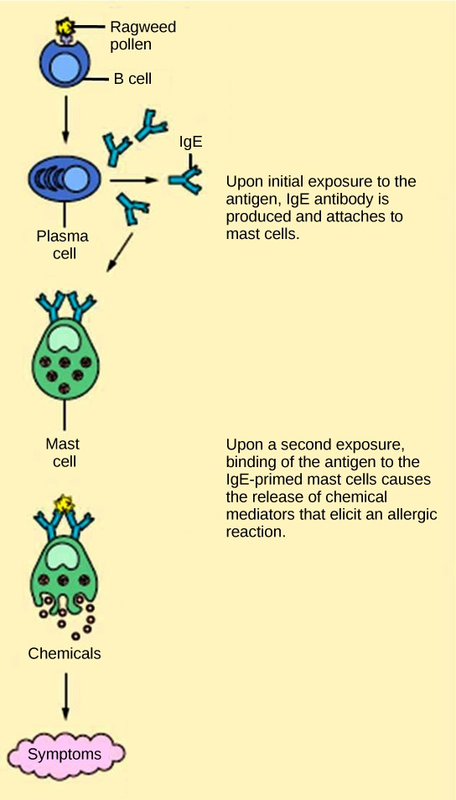
The immune reaction that results from immediate hypersensitivities in which an antibody-mediated immune response occurs within minutes of exposure to a usually harmless antigen is called an allergy. In the United States, 20 percent of the population exhibits symptoms of allergy or asthma, whereas
55 percent test positive against one or more allergens. On initial exposure to a potential allergen, an allergic individual synthesizes antibodies through the typical process of APCs presenting processed antigen to TH cells that stimulate B cells to produce the antibodies. The antibody molecules interact with mast cells embedded in connective tissues. This process primes, or sensitizes, the tissue. On subsequent exposure to the same allergen, antibody molecules on mast cells bind the antigen and stimulate the mast cell to release histamine and other inflammatory chemicals; these chemical mediators then recruit eosinophils (a type of white blood cell), which also appear to be adapted to responding to parasitic worms (Figure 17.22). Eosinophils release factors that enhance the inflammatory response and the secretions of mast cells. The effects of an allergic reaction range from mild symptoms like sneezing and itchy, watery eyes to more severe or even life-threatening reactions involving intensely itchy welts or hives, airway constriction with severe respiratory distress, and plummeting blood pressure caused by dilating blood vessels and fluid loss from the circulatory system. This extreme reaction, typically in response to an allergen introduced to the circulatory system, is known as anaphylactic shock. Antihistamines are an insufficient counter to anaphylactic shock and if not treated with epinephrine to counter the blood pressure and breathing effects, this condition can be fatal.
Delayed hypersensitivity is a cell-mediated immune response that takes approximately one to two days after secondary exposure for a maximal reaction. This type of hypersensitivity involves the TH1 cytokine-mediated inflammatory response and may cause local tissue lesions or contact dermatitis (rash or skin irritation). Delayed hypersensitivity occurs in some individuals in response to contact with certain types of jewelry or cosmetics. Delayed hypersensitivity facilitates the immune response to poison ivy and is also the reason why the skin test for tuberculosis results in a small region of inflammation on individuals who were previously exposed to Mycobacterium tuberculosis, the organism that causes tuberculosis.

Try your hand at diagnosing an allergic reaction by selecting one of the interactive casestudies (http://openstaxcollege.org/l/world_allergy)at the World Allergy Organization website.
- 2457 reads